Receiving health care as a sexual assault survivor: Who to tell and what to say — Part 1
Introductory note: This is the first in a two-part series about sexual assault. It addresses where to go and what to do if you’ve been sexually assaulted, and how to be in control of your own health care as a sexual assault survivor. Part 2 will examine the health care provider’s role in caring for sexual assault survivors.
When I was 19, something happened that changed the course of my life forever.
I was sexually assaulted.
My experience as a sexual assault survivor has shaped me as a nurse and a midwife, influencing the way I deliver care to women. I strive to respect their process of healing and work mindfully around the lingering triggers for trauma, just as I expect my providers to do for me.
Today I want to share my story as an assault survivor. Then I would like to share some tips on how to find good medical care if you have been sexually assaulted, because violence should never prevent women from accessing the best possible care that they need to live their lives.
My sexual assault story and how I became a survivor 
In 2007, my girlfriends and I spent spring break in West Palm Beach, Florida. It started out as a fun road trip, but it soon turned ugly. After going out one evening, I woke up in the middle of a stranger having sex with me. Stunned and confused (and pinned down), I laid awake in his bed for the rest of the night. When he woke in the morning, he tried to cuddle up to me and then made me breakfast. It was extremely confusing, but I now know that this is very common… rapists often make you breakfast. Some of my friends were in his living room, and when I told one of them that I had been sexually assaulted, she said, “Congratulations on losing your virginity!” I dug through every garbage can in the house looking for a used condom and found nothing.
I didn’t know what to do with myself, but I thought going to a clinic of some kind seemed like the right thing to do. This was a time before smart phones, and I didn’t exactly know how to get the information I needed. So, I drove around West Palm Beach with my friend scanning the sides of the road for any building that looked medical. I couldn’t find anything, and she was getting tired of looking, so I never had a sexual assault exam. I prayed I wasn’t pregnant as if that was the worst that could happen.
Upon returning home, I told my then-boyfriend what had happened and was full of shame since I had made such a big deal about keeping my virginity until marriage. His response was one of the worst that I heard: “Well, did he hold a gun to your head? No? Then it wasn’t rape.”
About two months after the sexual assault, I noticed something while taking a shower. I had genital warts. I must have cried and screamed in that bathroom for hours, breaking up with God and cursing all the people that had let me down. I had the worst breakdown of my life, but eventually I found some courage and went to a free clinic. An older, white, male doctor entered the exam room. I was so nervous and clammy, embarrassed and panicked about what he would say. When I explained that I had been sexually assaulted and contracted genital warts as a result, the doctor fulfilled my worst nightmare and replied, “Yeah, you and everybody else.” He refused to treat the warts and told me they would resolve on their own. The visit was five minutes long. I left that clinic in worse condition than when I entered.
Over and over, when I told the people who were supposed to support me, they downplayed my experience. No one validated me.

While the clinic did test me for STDs, I never got my results. No one bothered to call and tell me they were negative. Another two months passed, and I still woke up every day full of shame and the feeling of being dirty. I even sold back every single textbook I had a few weeks into the semester with intentions of dropping out of college. I partied with too much alcohol and isolated myself from my friends. I only slept during the day and stayed awake all night. Despite deep depression, I knew I couldn’t go on like this much longer. I tapped into my bravery reserves and went to the Student Health clinic at the University of South Carolina, where I was attending school. That appointment was another turning point in my life, but this time it was positive.
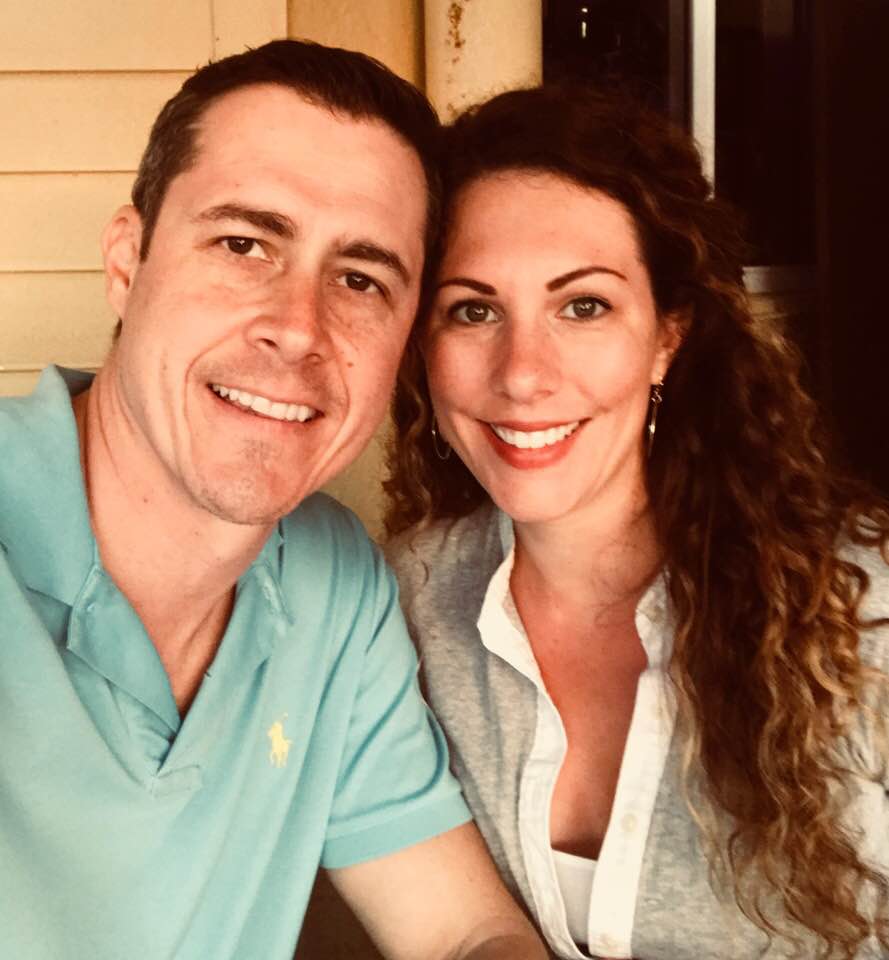
The Game Changer
I saw a nurse practitioner. She was young, like me. She had brown, curly hair, like me. Most importantly, when I told her what happened, she believed me. She spent time with me and gave me everything I needed. She treated my genital warts immediately without question and recommended support groups, even though I didn’t go to them. I wish I would have now! It might have saved me years of mental anguish. It may have prevented me from getting into a future serious relationship where sex was used as a weapon against me emotionally, spiritually, and physically. That’s another blog for another time.
She was amazing and is the main reason I am where I am now. After that appointment, I switched into the nursing program.
Side note: If anyone out there in the internet world knows of a nurse practitioner with brown, curly hair who was seeing patients at the University of South Carolina Student Health clinic in 2007, could you contact me? I would love to know her name and send her a card.
The reason I tell you this story is to break down the wall between patients and medical professionals — to let you know that health care providers are people, too. Sometimes, health care providers are even sexual assault survivors, like me.
Understanding sexual assault terminology and connotations
Before I completely dive in to the main topic of this post, I want to take a moment and address my choice of terminology. You have probably noticed that I prefer the phrase “sexual assault.” Why? Well, this is a highly sensitive topic, and the word “rape” can be inappropriate and triggering. Not always but often.
First, rape has connotations that reflect stories like mine — being taken by a stranger and forced to have sex without consent, sometimes accompanied by violence or injuries. Also, rape is a form of sexual assault, but not all sexual assault is rape. Some people don’t consider it rape if the act happens with an acquaintance, a friend, a boyfriend, or a husband. Sometimes those are downplayed to “misunderstandings”. Of course, that is not true; it is still rape. Some people prefer to use the term sexual assault because rape carries a heavy and often violent connotation. Sex without consent is rape, but that doesn’t mean it is the term we have to use. Survivors should use whatever terminology feels most appropriate to them.
Second, sexual assault is a more inclusive phrase. For example, it can describe any number of non-consensual sexual acts. Let us not forget that men can be sexually assaulted, and this term covers those cases, too. According to the Rape Abuse & Incest National Network (RAINN), the term “sexual assault” refers to sexual contact or behavior that occurs without explicit consent of the victim. Some forms of sexual assault include:
- Attempted rape
- Fondling or unwanted sexual touching
- Forcing a victim to perform sexual acts, such as oral sex or penetrating the perpetrator’s body
- Penetration of the victim’s body, also known as rape
Even as a sexual assault survivor and health care provider who is sensitive to other sexual assault survivors, I am not perfect. I am doing my best to heal and educate others. Please have grace with me and understand that I am still learning.
Seeking health care immediately after a sexual assault
The recommendation from the West Virginia Sexual Assault Forensic Examination (SAFE) Commission is to obtain care from a sexual assault nurse examiner (SANE) within 96 hours of the assault. A SANE will use a sexual assault evidence collection kit (SAECK). Sometimes called a “rape kit,” it is used to collect evidence that can be processed if a sexual assault survivor decides to report the crime to law enforcement. Pressing charges is optional, and there is no statute of limitations for sexual assault crimes in West Virginia. You can report a sexual assault to law enforcement at any time, but the unprocessed kits are kept for only two years and labeled “non-reports”. I would absolutely advise that if you are assaulted you should go get a kit done. You can decide what you want to do with it later. There are repercussions other than jail-time for perpetrators, such as expulsion from college or financial compensation.
In Monongalia County, the only place to receive care from a SANE is Ruby Memorial Hospital’s Emergency Department. However, if you are in another location or need care while traveling, your best bet is to go to any local emergency room. Be sure to request a SANE for the exam; they are specially trained to collect the best evidence and provide the most sensitive care. Even the most well-meaning clinicians can really screw up a sexual assault examination. Find someone certified to perform the exam. Find a SANE.
Speaking of evidence, one thing to keep in mind before receiving care for a sexual assault: Do not pee! If at all possible after a sexual assault, try not to pee until you get to an emergency room that will do a SAECK. If you can’t hold it or there is going to be a delay in health care, collect your urine and take it with you. There is so much DNA evidence that can be gathered from urine. Also, do not shower, change your clothes, or brush your teeth. I understand that this is the opposite of what you want to do after an assault. Lord knows the FIRST thing I did the morning after was take a long shower and attempt to wash away the memories of the night before. Let me save you the trouble and tell you that there aren’t enough showers in the world to wash that away. Save the evidence.
In addition to DNA evidence collection, one of the reasons for the 96-hour window for a sexual assault exam is because of physical injuries. Genital injuries heal very easily, so time is of the essence and photo evidence can help the case, if you choose to press charges.
Most importantly, please know that seeking health care after a sexual assault is so much more than a kit. You also get emergency contraception, HIV prophylaxis, treatment for sexually transmitted infections, and vaccinations for Hepatitis B, tetanus, and HPV, if appropriate. You can also receive medication to help you sleep and pain medication if there is physical injury. It will also flag you as a patient that needs follow up and possibly counseling. This way you won’t fall through the cracks like I did.
Receiving health care as a sexual assault survivor
As I mentioned, I did not have a SAECK done after I was sexually assaulted. Too much time had passed, but seeing a sensitive and well-trained nurse practitioner was life-changing.
If you are a sexual assault survivor who missed the 96-hour window, you can still — and should! — seek care. You can go to a primary care provider, an urgent care, or an outpatient clinic. A medical forensic exam would no longer be appropriate, but you can still be tested and treated for STIs.
Now, obviously as a Certified Nurse-Midwife, I believe wholeheartedly that regular well-woman care is important. But as a sexual assault survivor, I understand how difficult it can be to initiate that type of care and to keep up with it regularly.
If you have experienced sexual assault or abuse, it is important that you tell your health care provider — no matter how long ago it happened or how minor you perceive it to be. There are many studies in the works linking history of sexual assault to mental disorders, social issues, and physical health problems. We are barely scratching the surface in discovering how our bodies manifest trauma.
When scheduling your appointment, tell the office scheduler on the phone that you will require a longer appointment time. You can say something like, “I’m not willing to disclose what I’m being seen for, but there are things I would like to discuss that may take some time.” If the scheduler accommodates your request, that can potentially help you receive more sensitive and thorough care for your mind, body, and spirit. Having a provider who doesn’t feel rushed should make a big difference!
Trust me, it’s a terrible feeling to want to stay with a patient who you know needs your time and attention, but that means 20 other people will be waiting for extended periods of time. It’s one of the reasons I’ve chosen a business model that allows me to take my time and be in a non-triggering environment —a person’s home, although I do recognize there are instances when sexual assault occurs in a patient’s home. I accomodate as necessary.
It’s Not You, It’s Them
If your provider has a negative response to your bravery in opening up about your trauma, let him or her know your feelings. You can write it in an evaluation or tell them in person. If you don’t get what you’re looking for from a provider, it is not a reflection on you. Most importantly, get a new provider! Word of mouth is often the best way to find a provider who is sensitive and thorough with sexual assault survivors. Helpful resources and groups are listed at the end of the page.
In order to tailor your medical care appropriately, be honest and specific with me about your triggers before or during your appointment. Other providers may do this differently, but this is how I prefer to create a safe space for my patients. For example, if putting your legs in stirrups is a trigger, perhaps we can do the exam on your side. If you’ve had your breast groped and feel uncomfortable with a breast exam, I can show you how to perform the exam, and you can describe what you’re feeling. Depending on the screening, you may be able to swab yourself. In fact, we may not do anything physical at all during the first appointment. We can spend that first meeting discussing a plan of action for the next visit and learning relaxation techniques that can help achieve a less triggering appointment for you.
Even with all these options, there is something I want to make absolutely clear: Consent is a fluid relationship. If, at any point, a patient withdraws consent for any part of an exam, we’re done. It’s over. We will make a plan of action together and revisit whatever was missed the next time, or the time after that, or possibly never.
Takeaways about sexual assault and health care
As much as I encourage women to talk about their sexual assault and how it affects their health care, I realize it’s difficult. For many survivors, even ones whose trauma occurred years ago, it can feel like it happened yesterday. In fact, the assault may have happened in childhood and you literally do not remember it. Trauma can move to the non-verbal side of the brain and sit there for years unprocessed. Speculum exams and pap smears can trigger patients, and they may not even understand why. If you are feeling stressed at your appointment, I want to know about it. We can figure it out together.
As a Certified Nurse-Midwife, I often see patients who are completely fine for most of their appointment, but as we get closer to the speculum exam, I see their bodies physically change. I remember being in that position, laying on an exam table and thinking, “Please, just ask me.”
If I sense tension, I say, “I see you’re getting a little bit anxious about the speculum exam. Do you have a history of sexual assault?” The very last thing any provider wants to do is make something worse for you. Answering this question honestly will help us serve you with the best and most holistic care possible.
There are three messages I want every sexual assault survivor to know.
- It’s not your fault.
- You can heal.
- You’re not alone.

At Wise Women Health Care, I am honored to hear women’s stories. If you would like to learn more about my services and how I can tailor your care in a non-triggering way, please contact me. You can text 304-449-6670 for an appointment. Or click, HERE.
Helpful Resources:
Rape & Domestic Violence Information Center
WVU Students- Information on Sexual Assault
Information for Victims to Connect
Rape, Abuse, & Incest National Network
Trauma-Sensitive Therapist in Morgantown, WV
WV Foundation for Rape Information Services
